The National Health Care Anti-Fraud Association estimates that health care fraud costs our country approximately $68 billion a year! Medical billing fraud rests under the health care fraud umbrella and is responsible for millions of the fraud dollars lost each year. Keep reading to learn more about medical billing fraud.
Health care fraud affects everyone. It can be committed by health care professionals, patients, and others who intentionally deceive the health care system to receive unlawful benefits and payments. The effects of health care fraud include higher health care premiums, increased taxes, and exposure to unnecessary procedures.
One aspect of health care fraud is medical billing fraud.
Medical Billing Fraud
Medical billing fraud is the misrepresentation or misstatement of facts about the scope, the type, or the nature of a medical treatment or service provided, in a manner that could result in unauthorized payments. More simply, medical billing fraud is using deceptive tactics through medical paperwork to reap unwarranted money.
There are three common types of medical billing fraud. They include:
Upcoding Fraud: This occurs when a medical professional sends a bill to Medicare or another payor for a more expensive service than the one actually performed. Examples of this include:
- Exaggerating the amount of time a medical procedure took to complete
- Lying about the number of medical professionals were part of the procedure
- Making up a procedure that never occurred
- Violating “medical necessity” rules and performing procedures that are unneeded
Unbundling Fraud: According to the FBI, unbundling is “…the practice of submitting bills in a fragmented fashion in order to maximize the reimbursement for various tests or procedures that are required to be billed together at a reduced cost.”
An example of unbundling medical billing is when a provider illegally uses separate codes for routine surgery. They might use unique codes for incision and suturing instead of using the appropriate billing code with a lower reimbursement rate. Unbundling is basically charging more for each part of a specific procedure when a lower rate for the entire procedure exists.
Phantom Billing: To be covered by insurance, or Medicaid, the billed service or supply must be provided. Some providers bill Medicaid for a covered service or item but do not deliver the service or item. These providers may create false records in an attempt to justify the bills.
One example of phantom billing would include a physician signing charts and submitting bills for examinations that never occurred. Another example could be a diagnostic testing lab submitting a bill claiming it performed both a 2D CAT scan, as well as a sophisticated 3D scan, when really it only completed the 2D scan.
These examples of medical billing fraud represent only a portion of health care fraud. Being accused of any of these crimes is a serious charge.
How is Medical Billing Fraud Prosecuted in New Jersey?
Medical billing fraud is a Federal offense and in New Jersey is investigated by the Federal Bureau of Investigations (FBI), the Office of Inspector General (IOG), the New Jersey Medicaid Control Unit (MFCU), and prosecuted by Assistant United States Attorneys from the U.S. Attorney’s Office in Camden, Trenton, or Newark.
New Jersey also established the New Jersey Healthcare Claims Fraud Act (NJHCCFA) to address this type of fraud. A primary concern of this act is to prevent false claims from being filed with insurers for medical products or services that were not received or performed.
One more line of defense against health care fraud in New Jersey is the New Jersey Fraud Detection Program. If someone has knowledge of what they believe to be health care related fraud, they can call an “insurance fraud hotline” that operates 24 hours a day. The Attorney General may pay up to $25,000 for information leading to a health care fraud conviction.
There are many ways the State of New Jersey works against health care fraud. Being accused and convicted of this type of crime in New Jersey can also lead to serious consequences.
What are the Penalties for Medical Billing Fraud in New Jersey?
Again, because medical billing fraud is a Federal offense, the penalties for committing it are harsh. This is especially true if you are found guilty of defrauding Medicaid, a government-run program.
Prison sentences of up to three years are common for these offenses, as well as hefty fines and professional ruin. If you are convicted of healthcare fraud in New Jersey, the fine is often five times the value of the false claim you attempted to file. For example, if the false claim was for $25,000, you could pay a fine of $125,000 if convicted of fraud.
What Should I Do if I’m Accused of Medical Billing Fraud?
Facing the consequences of a health care fraud conviction in New Jersey has the potential to be life-altering. It’s important that you find a criminal defense attorney that is experienced in this type of defense and has the skill to work on your behalf against the professionals that work for the government.
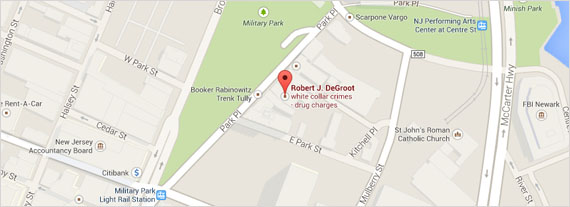
If you or someone you know is facing a medical billing fraud accusation, reach out to the Law Offices of Robert J. DeGroot for advice and assistance!