When medical billing is done correctly, it ensures that medical services are billed using industry standards and reduces the possibility of fraudulent billing practices.
The Correct Code
Medical coding is one of the most important aspects of the healthcare industry. Medical codes translate patient information into a universal alphanumeric language that can be understood by insurance companies and other medical professionals.This information is used to track payments and generate bills, as well as maintain precise medical records. With changes in the healthcare industry, like the Affordable Care Act, medical coding has become even more important.
The importance of medical coding was realized as more and more electronic transactions between providers and insurers started taking place. As these transactions increased, so did inefficiency and confusion because of the different ways transactions were being handled. Congress required the adoption and use of national standards overseeing the nature and content of electronic transitions in healthcare. This act is known as the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
HIPAA regulations are in place to protect everyone involved in a healthcare transaction, from the patient to the provider to the insurer. Protected Health Information (PHI) breaches have affected over 176 million patients in the United States. Most of these breaches resulted from employees’ negligence and noncompliance with HIPAA regulations rather than outside hacking. This is why the accuracy of medical coding is so important to the protection of valuable healthcare and financial information.
How Medical Coding Protects Against Fraud
Healthcare fraud is an issue that negatively impacts the integrity of the healthcare industry and results in the loss of billions of dollars each year. In fact, last year in the United States just under 200 defendants were prosecuted for healthcare fraud with intended losses exceeding $2.75 billion. Those are just the cases where legal action was taken, many more billions are lost to fraud in actions that are not discovered.
Healthcare fraud involves deception or misrepresentation with the intent to receive unauthorized benefits. Common forms of healthcare fraud include:
- Billing for Services Not Rendered: Submitting claims for services, procedures, or equipment that were never provided.
- Upcoding: Billing for more expensive services or procedures than what was performed.
- Unbundling: Billing procedures or services separately that should be billed together under one code.
- Kickbacks: Offering or accepting payments in exchange for patient referrals or services.
- Phantom Billing: Charging for non-existent medical services or supplies.
Medical coding is essential to eliminating fraud. Its focus on compliance regulations, detailed universal codes, and maintaining an organized system all help to protect against, and detect, fraudulent activity.
Combatting Healthcare Fraud with Medical Coding
Medical coding exists to protect anyone involved with the healthcare industry, which means medical coding protects every citizen at some point in their life.
Ensuring that healthcare workers are paid for the services they provide is important to maintaining a functioning healthcare system. Patients are also protected by medical coding by guaranteeing accurate record keeping and billing, and maintaining patient privacy. Insurers are also protected by medical coding by confirming accurate claim submissions, preserving compliance, and reducing the risk of fraud.
Key practices that medical coders follow to establish trusted and detailed medical records include:
Exact Documentation: All aspects of patient care are documented from time and date of appointments to services and procedures provided.
Use of Correct Codes: Confirming that all codes used reflect the actual services provided as well as the patient’s diagnosis.
Awareness of Billing Guidelines: Knowledge of how each insurer, including Medicare and Medicaid, bills for services rendered is important. Submitting claims on time and making sure that services that can be bundled together are placed under the correct code.
Compliance Checks: It’s vital that regular internal audits are done to ensure accurate practices.
These key practices check for discrepancies and provide a safety net against committing fraud. Healthcare fraud can have severe consequences and negatively impact many lives.
Consequences of Healthcare Fraud
Fraudulent medical coding or billing practices can have detrimental consequences for healthcare providers, patients, and the overall healthcare system. Fraud is not taken lightly by the justice system in the United States, and lives can be changed forever because of it. The repercussions of healthcare fraud include financial, legal, and professional ramifications.
Legal Outcome
The U.S. Department of Justice (DOJ) and the Department of Health and Human Services (HHS) assertively prosecute cases of healthcare fraud. A conviction can result in hefty fines, restitution, and a prison sentence.
Financial Outcome
The financial downfall from a healthcare fraud conviction can be severe. Repayment of funds, civil fines, and loss of reimbursement privileges can be enough to wipe out an individual’s net worth. Not being able to bill Medicare or Medicaid puts a major stress on any medical provider’s stream of revenue.
Professional Outcome
The professional effects of a healthcare fraud conviction can result in the loss of one’s medical or professional licenses. This could mean the end of a career. The loss of reputation is also important to consider as a loss of trust can result in a loss of patients.
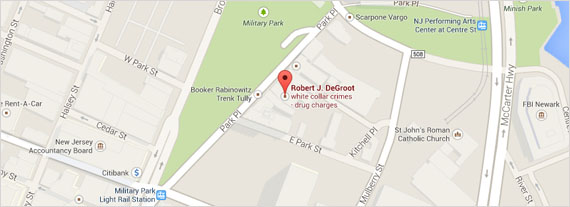
Medical coding works to prevent fraud from occurring. If you are accused of fraud, it is imperative to seek the help of an experienced defense attorney, like the legal team at the Law Offices of Robert J. DeGroot.
Reach out to the Law Offices of Robert J. DeGroot if you or someone you know has been accused of healthcare fraud.