Medicare and Medicaid fraud costs taxpayers over $100 Billion a year. Imagine what you could do with $100 Billion–purchase all of the NFL and MLB teams in the country, save the Great Barrier Reef, or even buy your own country! Knowledge of Medicare and Medicaid fraud, and what to do if you’re convicted of it, could make a huge difference in your life.
The Difference Between Medicare and Medicaid
Medicare is federal health insurance for anyone age 65 and older, and some people under 65 with certain disabilities or conditions. Medicaid is a joint federal and state program that gives health coverage to some people with limited income and resources.
People on Medicare pay part of their costs through things like monthly premiums for medical and drug coverage, deductibles and coinsurance. People with Medicaid generally do not pay anything for covered medical expenses, but may owe a small co-payment for some items or services.
Medicare & Medicaid Fraud
What is Medicare & Medicaid Fraud?
Medicare and Medicaid fraud occur when individuals or organizations knowingly submit false claims to Medicare or Medicaid for reimbursement. This can include billing for services or supplies that were never provided, billing for services that were medically unnecessary, or receiving kickbacks for referring patients to certain providers.
How Is Medicare & Medicaid Fraud Committed?
Medicare and/or Medicaid fraud can be committed by a variety of individuals and organizations, including healthcare providers, suppliers, and even patients. Some common methods of Medicare and Medicaid fraud include:
- Upcoding: This involves billing for a more expensive service than was actually provided.
- Unbundling: This involves billing separately for services that should be billed together as a package.
- False certification: This involves billing for services that were not actually performed by a licensed healthcare provider.
- Kickbacks: This involves receiving payment for referring patients to certain providers or suppliers.
- Phantom billing: This involves billing for services that were never provided.
Why is Medicare and Medicaid Fraud a Problem?
Medicare and Medicaid fraud is a significant problem for several reasons. First, it costs taxpayers billions of dollars each year. According to the National Health Care Anti-Fraud Association, taxpayers are losing more than $100 billion a year to Medicare and Medicaid fraud.
Fraudulent activities can also harm patients by providing them with substandard care or services they don’t need. For example, a patient may be prescribed a medication they don’t need or undergo a surgical procedure that is unnecessary. These activities can also lead to higher healthcare costs and reduced access to care for patients who truly need it.
What Are the Penalties for Medicare and Medicaid Fraud?
Medicare and Medicaid fraud are serious crimes that can result in severe penalties. Healthcare providers who engage in fraudulent activities can face fines, imprisonment, and exclusion from Medicare and Medicaid programs. Providers may also be required to pay restitution to the government.
Patients who engage in fraud can also face penalties. For example, a patient who accepts a kickback for receiving treatment may be charged with a crime.
What To Do if You’re Convicted of Medicare or Medicaid Fraud
Being convicted of Medicare or Medicaid fraud is a serious crime with serious consequences. If you find yourself in this situation, it’s important to take immediate action to protect your rights and minimize the impact such a conviction may have on your life. Here are some things to consider if you’re convicted of Medicare or Medicaid fraud:
- Hire an experienced attorney
The first thing you should do is hire an experienced attorney who specializes in healthcare fraud cases. A knowledgeable attorney can help you understand your legal options and develop a strategy to defend your case.
- Cooperate with investigators
Cooperating with investigators is crucial if you’re convicted of Medicare or Medicaid fraud. Failing to cooperate can result in additional charges and penalties. Your attorney can help you navigate the investigation process and ensure that your rights are protected.
- Prepare for sentencing
If you’re convicted of Medicare or Medicaid fraud, you will be sentenced by a judge. It’s important to prepare for sentencing by gathering evidence that supports your case and demonstrating your willingness to make restitution for any damages caused by the fraud.
- Explore your options for appeal
If you’re convicted of Medicare or Medicaid fraud, you may have the option to appeal the decision. Your attorney can help you evaluate the strength of your case and determine whether an appeal is a viable option.
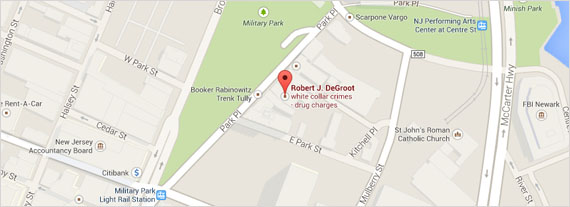
If you or someone you know has been convicted of Medicare or Medicaid fraud, finding an experienced attorney to discuss your options with should be your first move–the Law Offices of Robert J DeGroot specializes in criminal defense law and can help. Reach out to us today for a free consultation.